Full-arch fixed prostheses (eg, All-on-X) have become very popular in implant dentistry today. There is an abundance of literature discussing complications with this type of prosthesis, such as fractures, hygiene and aesthetic issues. A significant complication that may be devastating, yet often overlooked, is speech or phonetic issues. Various clinical studies have reported a high prevalence of speech issues with fixed implant prostheses; Collaert et al1 reported that 84% of patients with full-arch fixed implant prostheses exhibited one or more pronunciation errors after 6 years, Bothur and Garsten2 concluded 83% of patients receiving implant prostheses had generalized speech problems, and Van Lierde et al3 reported that more than 87% had at least one consonant phonetic deficit. Therefore, to minimize the possibility of postoperative speech and phonetic problems, clinicians must have a strong understanding of the physiologic effects that full-arch implant prostheses may have on speech.
In the re-establishment of dental health for edentulous patients, mechanics, aesthetics, and speech maintenance are important principles that must be evaluated. Unfortunately, many clinicians do not place emphasis on the design and type of prosthesis with respect to its impact on the speech process. The ability to pronounce various phonetic sounds is dictated by the position and musculature of the tongue.4 If the tongue is impeded by the design of the prosthesis in any way, patients may have difficulty pronouncing certain phonetic sounds.
There exist many reasons why patients exhibit speech problems after full-arch implant treatment:
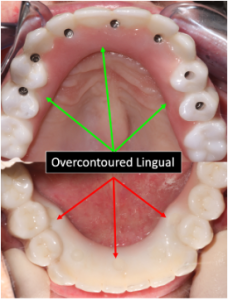
1. Overbulked prostheses. After teeth are lost, the natural bone resorption process usually will result in the loss of existing hard and soft tissue. This most commonly will lead to a final implant prosthesis that is larger (overbulked) in the vertical and horizontal planes. Initially, because the prosthesis is foreign to the patient, the alteration of speech sounds often results. This is directly related to the inability of the tongue to freely move because of the impingement of the prosthesis (Figure 1).
Figure 1. (a) A maxillary prosthesis depicting overcontoured lingual contours. (b) A mandibular prosthesis showing lingually positioned implant positions, resulting in a lingually overcontoured prosthesis. Both of these prostheses will prevent free movement of the tongue for ideal articulation.
Figure 2. Macroglossia resulting from mandibular edentulism and the lack of an interim prosthesis.
Figure 3. Multiple air spaces resulting from tissue recession.
2. Macroglossia (enlarged tongue). The tongue is the most important articulator of speech sounds and is controlled by 8 different muscles classified as intrinsic and extrinsic. The intrinsic muscles allow the tongue to change shape, and the extrinsic muscles act to modify the position of the tongue.4 When teeth are lost, these muscles are directly affected, which results in alteration of speech. In addition, the tongue may increase in size (macroglossia), especially if an interim prosthesis is not worn. The enlarged tongue is problematic for patients when adapting to an implant prosthesis as patients often complain inadequate room exists for proper articulation (Figure 2).
3. Prosthesis adaptation. The most common dental materials used today for full-arch implant prostheses include zirconia, porcelain-fused-to-metal, and acrylic. Because these materials are “foreign” to the patient, patients will often have difficulty adapting to the prosthesis, which may result in speech difficulties. In addition, these prostheses are often heavier than conventional prostheses, which further complicates the prosthesis adaptation process.
4. Loss of proprioception. When teeth and their associated soft tissues are lost, the proprioceptive feedback system is often altered. The fine motor movements in the oral cavity are dictated by the teeth and their associated structures. Therefore, because speech is an unconscious act, the loss of the proprioceptive mechanism may result in the patient having difficulty in tongue control and producing various speech sounds.
5. Prosthesis air spaces. The design of the prosthesis, especially in relation to the intaglio surface, may lead to speech difficulties. Embrasure spaces are an integral part of allowing for proper post-op hygiene maintenance. Most commonly found in the maxillary arch, space present between the tissue and the prosthesis may allow air and saliva to flow through the openings, causing speech issues (Figure 3).
PHONETIC COMPLICATIONS
In the process of recording maxillomandibular records for patients, it is imperative that the clinician understands the relationship between the prosthesis and the tongue, teeth, and lips. Initially, many full-arch fixed implant patients have difficulty pronouncing consonant sounds. The following are examples of specific consonant sounds that are affected by a final implant prosthesis.
1. “F” and “V” (labiodental sounds). The sound generation of the labiodental sounds (“F” and “V”) occurs directly from forced air between the maxillary incisal edges (anterior) and the lower lip. These specific sounds are important in determining the occlusal plane and the anterior-posterior positioning of the maxillary incisors. Ideally, the maxillary incisal edges should slightly contact the vermillion border of the lower lip in the pronunciation of these sounds. When the maxillary anterior incisal edges are positioned too “long,” “F” sounds will often be pronounced as “V” sounds. If the maxillary anterior incisal edges are too “short,” “V” sounds may be articulated as “F” sounds. These sounds are also directly affected by the occlusal plane. If the occlusal plane is positioned too high, relaxation of the lips will be impaired. If the occlusal plane is positioned too low, the lower lip will overlap the maxillary incisal edges, which will result in strained speech sounds5 (Figure 4a).
2. “S,” “Z,” “SH,” and “ZH” (sibilant sounds). The “S” sounds (and also “Z,” “SH,” and “ZH” sounds) are generated when the tongue is moved anteriorly toward the roof of the mouth, coming very close to the anterior teeth without making contact. A “hissing” sound is formed by air being pushed past the tongue. Often, because of non-ideal implant positioning in the premaxilla, these sounds are directly affected due to an overbulked anterior region. In addition, the premolar area may be bulky, which may obstruct the tongue, preventing air from escaping and resulting in a whistling sound. In the pronunciation of “S” sounds, lisping may occur if the palatal part of the implant prosthesis is too thick or if a lack of freeway space is present (Figure 4b).
3. “TH” and “L” (linguo-dental sounds). The linguo-dental sounds are produced when the tip of the tongue passes between the anterior incisal edges in very slight contact with the maxillary teeth (lingual). In the establishment of the labiolingual position of the anterior teeth, these sounds are often used. In ideal positioning, approximately 3 mm of the tip of the tongue should be seen when pronouncing the linguodental sounds. If less than 3 mm of the tongue tip is seen, the position of the teeth is too far forward (excessive vertical overlap). When more than 6 mm is seen, the maxillary teeth are positioned too far lingually6 (Figure 4c).
4. “B,” “M,” and “P” (bilabial sounds). The “B,” “M,” and “P” sounds are produced when the upper and lower lips come into contact. The “P” and “B” sounds are pronounced with an explosive effect. “M” sounds are produced with a more passive effect. These sounds are commonly used in establishing the ideal vertical dimension. When the vertical dimension is too open, inadequate freeway space will be present, and the lips will have difficulty contacting each other. When lip strain is present, the bilabial sounds will be distorted (Figure 4d).
5. “D,” “N,” and “T” (tongue to anterior lingual teeth sounds). The “D,” “N,” and “T” sounds are generated when the tip of the tongue contacts the maxillary lingual tooth surfaces and the anterior palate (incisive papilla). An explosive sound is formed when the tongue is drawn downward after contacting the lingual area. D, N, and T are termed “plosive” consonants. These sounds are often difficult to articulate because of an overcontoured lingual prosthesis, which results from a lingual-oriented implant position in the premaxilla (Figure 4e).
PREVENTION
To minimize the possibility of post-op phonetic complications, the following may be implemented:
1. Detailed informed consent. The patient should be educated, both verbally and in writing, on exactly what type (eg, design, shape, and size) of prosthesis he or she will be receiving. The use of prosthesis patient models made from the type of prosthesis material to be used (eg, zirco- nia, porcelain/metal, or acrylic) is an ideal way to convey the final prosthesis type.
In addition, the patient should be instructed on expectations and an adaptation period, which will reduce any possible misconceptions.
2. An interim prosthesis. After tooth removal, it is crucial that patients wear an interim prosthesis, even for a short period of time during the day. Because of the loss of proprioception and muscle control after tooth loss, speech may be affected. In addition, the vertical dimension of occlusion, centric occlusion, increased muscle atrophy, and tongue enlargement (macroglossia) may be altered or lost if no interim prosthesis is worn.
3. Post-op exercises. The tongue must have sufficient time to adapt to the new implant prosthesis. The easiest technique to allow for patient adaptation is to instruct patients on the use of musculature and phonetic exercises. An ideal exercise plan includes instructing patients to speak or read out loud, usually with a book or magazine, for 30 minutes twice a day. It is highly variable how long it can take a patient to adapt to a prosthesis.
IN SUMMARY
Since the early days of the Brånemark fixed hybrid prosthesis, many advances in implant technology have developed. However, patient education is very important as patients have far greater expectations today than in the past. Therefore, it is imperative that the implant clinician educates the patient on the adaptation phase of full-arch implant prostheses and the importance of proper speech articulation. Speech articulation is a complex component and an often-misunderstood part of the implant process. When a full-arch implant prosthesis is inserted, the goal is not only to restore function and aesthetics but also to maintain proper patient phonetics. Ideally, this may be accomplished by having the patient wear an interim prosthesis that closely parallels the patient’s original maxillomandibular measurements and through the use of post-op phonetic exercises.
REFERENCES
1. Collaert B, Van Dessel J, Konings M, et al. On speech problems with fixed restorations on implants in the edentulous maxilla: introduction of a novel management concept. Clin Implant Dent Relat Res. 2015;17 Suppl 2:e745–50. doi:10.1111/cid.12309
2. Bothur S, Garsten M. Initial speech problems in patients treated with multiple zygomatic implants. Int J Oral Maxillofac Implants. 2010;25(2):379–84.
3. Van Lierde K, Browaeys H, Corthals P, Muss- che P, Van Kerkhoven E, De Bruyn H. Comparison of speech intelligibility, articulation and oromyofunctional behaviour in subjects with single-tooth implants, fixed implant prosthetics or conventional removable prostheses. J Oral Rehabil. 2012;39(4):285–93. doi:10.1111/j.1365-2842.2011.02282.x
4. Liddelow FG. Clinical dental prosthodontics: Phonetics. Butterworth and Co. Ltd.;1989:136-139.
5. Pound E. Utilizing speech to simplify a personalized denture service. 1970. J Prosthet Dent. 2006;95(1):1-9. doi:10.1016/j. prosdent.2005.10.004
6. Chaturvedi S, Gupta N, Tandon A. Speech considerations. J Dental Med Sciences.2015;14(17):34-36.